
Barnes-Jewish Hospital, in partnership with WashU Medicine physicians, brings together a multidisciplinary team of specialists from orthopedics, plastic and reconstructive surgery, and neurosurgery, who collaborate on the treatment and repair of peripheral nerve injuries. Supported by state-of-the-art facilities, and a dynamic research environment, WashU Medicine experts have a long history of developing groundbreaking techniques and treatments for nerve repair. They continue to advance the science of nerve surgery through innovative surgical techniques and by improving outcomes for patients with complex nerve injuries.
Among them are WashU Medicine orthopedic surgeons, David Brogan, MD, MSc, and Christopher Dy, MD, MPH, who are pioneering new approaches to treating brachial plexus injuries, including those caused by high-velocity trauma such as motor vehicle accidents.
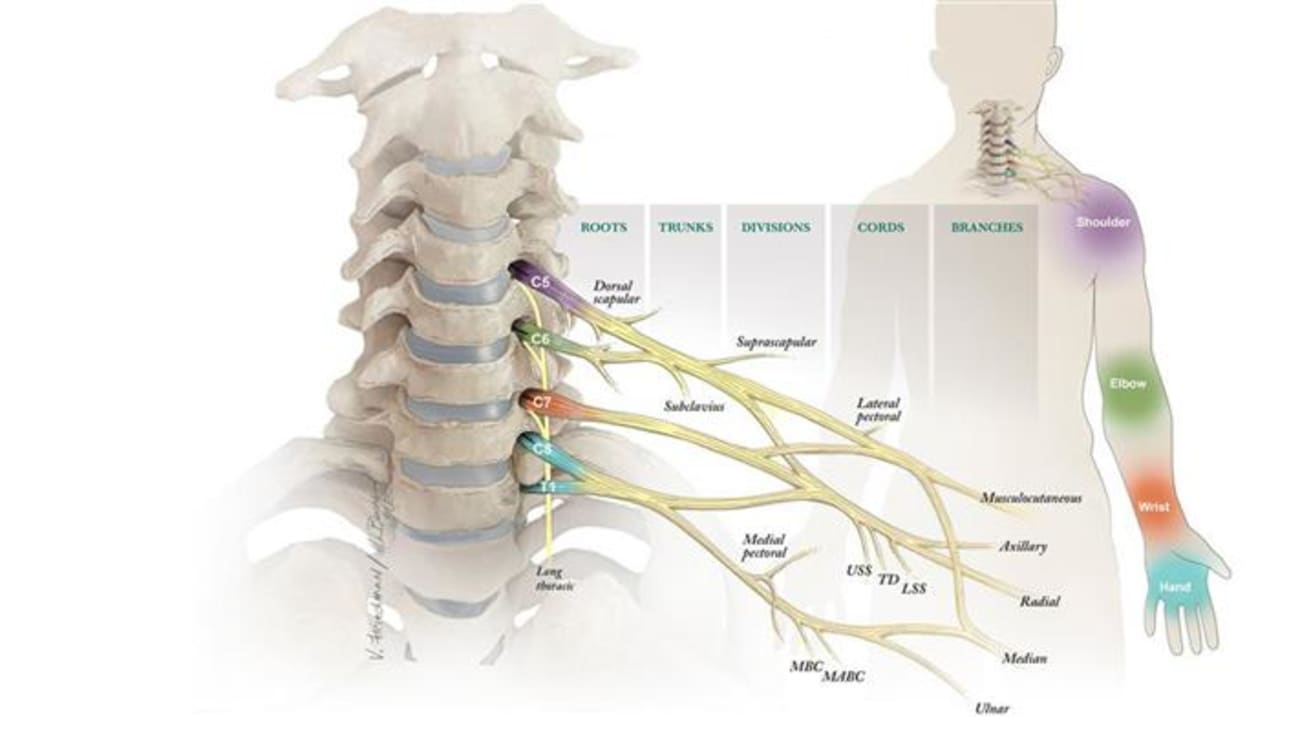
Brachial plexus injuries occur when the network of nerves that control muscle function and sensation in the shoulder, elbow, and hand is damaged. These injuries often result from trauma that forces the shoulder downward while the head is pushed upward, stretching, or even tearing the delicate nerve fibers. Injuries to this nerve bundle can result in devastating outcomes, from weakness to complete paralysis of the arm, depending on the location and severity of the damage.
Both Dr. Brogan and Dr. Dy are microsurgical-trained hand surgeons who specialize in hand surgery and peripheral nerve injuries.
The study of brachial plexus injuries goes beyond the operating room. It’s a blend of leading-edge science, global collaboration, and a deep understanding of the human side of trauma.
“These injuries are often overlooked in the early trauma workup,” says Dr. Brogan. “But the earlier we see these patients, ideally within a few weeks after their injury, the better the chance we have at restoring meaningful function.”
WashU Medicine orthopedic specialists at Barnes-Jewish Hospital are distinguished not only by their clinical expertise, but also by their integrated, multidisciplinary approach. Orthopedic surgeons collaborate with specialists including neurologists, rehabilitation specialists, and mental health providers, and the care team is structured to support the patient’s recovery from every angle—physical, functional, and emotional.
“What makes our program unique is how we integrate the science and the psychosocial journey of each patient,” Dr. Brogan continues.
Both Dr. Brogan and Dr. Dy are involved in the scientific and clinical aspects of care. Dr. Brogan’s research focuses on the basic science of nerve regeneration, while Dr. Dy concentrates on measuring and optimizing outcomes to address both physical and emotional factors throughout the patient’s journey.
“As orthopedic surgeons, we’re trained to focus on what we can fix,” says Dr. Dy. “But that’s just one part of it. We’re learning to see the whole picture—what this injury does to a person’s identity, to their mental health, and to their family. It can take months to see improvement, and if we catch it late, patients are scared and frustrated. But when we see them early, outcomes are better, and they feel less alone.”
Leading with precision and purpose
Dr. Brogan and Dr. Dy are exploring ways to improve nerve regeneration and muscle recovery. On the research front, the program is breaking new ground in both clinical and translational science. Ongoing clinical studies are exploring techniques to enhance nerve regeneration, including intraoperative electrical stimulation and polyethylene glycol (PEG) fusion, an experimental method aimed at reconnecting severed nerve fibers to speed recovery.
From research to real-world application, the surgical options provided by WashU Medicine physicians at Barnes-Jewish Hospital are among the most advanced in the St. Louis region.
“Both Dr. Dy and I see and assess the patients,” Dr. Brogan says. “In surgery, we explore the plexus, identify which nerves can be repaired or transferred, and determine what strategies will give that patient the best chance at regaining function.”
Among the most advanced techniques offered at Barnes-Jewish Hospital is free-functioning muscle transfer, a procedure in which muscle is taken from another part of the body, such as the leg, and transplanted into the arm to restore lost motion. “We’re also using vascularized ulnar nerve flaps and intercostal nerve transfers, depending on what the patient needs,” says Dr. Brogan. “There are only a few of us in the Midwest doing free-functioning muscle transfers at this level, and we’ve seen promising results.”
The work doesn’t stop in the United States. “We’ve built a global network of collaborators, including surgeons in Taiwan, England, and France,” Dr. Brogan says. “While it’s too early to share outcomes with vascularized ulnar nerve grafts from our patients, the international data has been very encouraging.”
“Everything we’re doing is about improving the time to diagnose, the quality of the repair, and ultimately, the patient’s quality of life,” says Dr. Brogan. “These are usually quite disabling injuries and the ability to help someone with a devastating problem in a time of great need is truly a privilege and something that I find quite rewarding.”
More than a physical injury
For many patients, a brachial plexus injury isn’t just a physical setback. It’s a life-altering event.
“Recovery from these injuries isn’t just about nerve repair—it’s about treating the whole person,” says Dr. Dy. “Pain management, psychological support, and guided rehabilitation are essential to maximizing long-term outcomes. This is a devastating injury, something very similar to a spinal cord injury, but isolated to the arm,” says Dr. Dy. “It affects a lot of people in the prime of their lives who are trying to support families. Many of them rely on their hands for their jobs. And when you lose the use of a hand, arm, and shoulder, and the sensation can possibly go with it, your entire life can change.”
According to Dr. Dy, it’s not uncommon for patients to suffer emotionally and financially.
“We interviewed 20 brachial plexus patients in St. Louis to better understand their journey,” says Dr. Dy. “Some patients become homeless because of this. Some lose their jobs. Others go through divorce. It was clear many felt lost in the process. They didn’t know what to expect or when. It was humbling, both as a physician and as a person, to learn what they’ve been through.”
Out of those interviews came new tools: a National Institute of Health (NIH)-funded patient education guide developed with input from a medical librarian from Becker Medical Library, a hand therapist, and a pain management expert. “We added illustrations and made it something we use in the clinic with our patients. And we built a patient-facing website so other surgeons can provide the information to their patients.”
“We also conducted a photojournalism project called PhotoVoice, inviting brachial plexus patients to take photos responding to questions such as, ‘How does pain interfere with your life?’ and ‘What hacks help you live with the use of one arm?’
“It was incredibly moving seeing their photos and stories,” he continues. “I now share some of those with other patients. It helps them see they are not alone and that there is life after this injury.”
Recognizing how overwhelming the journey can be, Dr. Dy recently secured a grant from The Foundation for Barnes-Jewish Hospital to add a patient navigator. “Patients need more than surgery,” says Dr. Dy. “They’re asking, ‘Who can help me? How do I get on Medicaid? How do I get to my appointments?’ The navigator helps with all those details.”
The team’s approach is more than surgery—it’s about rebuilding lives. “This is rewarding and life-changing work,” says Dr. Dy. “We’re doing everything we can, clinically and scientifically, to help patients regain function, confidence, and hope.”
With a commitment to improving function and quality of life for patients affected by brachial plexus injuries, WashU Medicine orthopedic specialists at Barnes-Jewish Hospital remain at the forefront of nerve repair science and clinical care.
Early consultation can have a great impact on long-term outcomes for patients with brachial plexus injuries. To learn more about how to refer your patients to a WashU Medicine orthopedic specialist, call 314-996-8970 or visit us online.



